Introduction:
Severe head injuries tend to be associated with hypermetabolism and hypercatabolism resulting in negative nitrogen balances which may exceed 30 grams/ day5. That is why early nutrition is very important. Once the patient has been fluid resuscitated and stabilized on declining doses of <2 vasopressors, EN may be started cautiously at low rates1. EN should be administered within 24–48 h once the patient is stable with vasopressors1. The ASPEN and ADA EBGs recommend enteral feeding should be started early, within the first 24–48 hours of admission, and advanced toward optimal nutrition goals over the next 48–72 hours2. Continuous intragastric feeding and initiating adequate nutrition within 72 hours of injury are recommended by the AANN to improve feeding tolerance and outcomes, respectively3. The Brain Trauma Foundation guidelines emphasize the need for feeding at least by the end of the first week post injury, and indicate that feeding prior to seven days improves outcomes4.
Calories should be in range of 25-30 Kcal/kg body weight/day for most critically ill patients1. Protein requirement for most critically ill patients is in range of 1.2-2.0 g/kg body weight/day1. In severely hypercatabolic patients such as extensive burns and polytrauma, ratio of Kcal: nitrogen should be 120:1 or even 100:1 has been accepted1. If it is apparent that the gastro-intestinal tract cannot be used to reach the nutritional goals within three days, total parental nutrition is begun within 24-48 h so as to reach these nutrition goals by either one or both routes by the third or fourth day5.
Indirect calorimetry to determine the respiratory quotient and resting energy expenditure should be determined twice weekly5. To determine N2 balance, urinary urea nitrogen should be measured in 24-h specimens. These tests should be performed once or twice weekly until it is clear that the nutrition is adequate5.
Though there are many guidelines for these patients but implementation is very important. In actual scenario there is a big gap between required and given nutrition due to many factors. It is very imp to recognize these factors and try to remove or overcome these problems for giving full nutritional support to the patients.
This study was conducted to evaluate nutritional intake of head injury patients admitted in a hospital.
AIM:
To Identify appropriate Nutrition Care Plan strategies for the maintenance and support of optimal nutrition status as per international standards.
OBJECTIVE:
- To assess the time duration of first feed from admission.
- To assess the Nutritional support/consumption in first 24 hours to 7 days and total days of NPO in first 7 days of head injury patients.
- To identify the barriers in implementing of standard protocol and improve the compliance rate.
SAMPLE: 100 (All head injury patients)
DURATION OF AUDIT: 1ST Nov 2017 to 31st July 2018
- Pre – Audit:
- Sample: 81
- Time Period: 1st Nov 2017 to 31st May 2017
- Analysis Period: 1 June to 15 June
- Post-audit :
- Sample: 19
- Time Period: 15 June to 31 july
INCLUSION CRITERIA :
- Only head injuries patients
- No contra indication
EXCLUSION CRITERIA:
- LAMA (leave against medical advice) Patients
- Age Below 16 Years
- Dead Patients
| 1 | Name | ||||||||||||||||
| 2 | MRN | ||||||||||||||||
| 3 | Age | ||||||||||||||||
| 4 | Gender | ||||||||||||||||
| 5 | Height | ||||||||||||||||
| 6 | Weight | ||||||||||||||||
| 7 | BMI | ||||||||||||||||
| 8 | Diagnosis/ complications | ||||||||||||||||
| 9 | Date of Admission | ||||||||||||||||
| 10 | Time of Admission | ||||||||||||||||
| 11 | Date of Discharge | ||||||||||||||||
| 12 | Total no of Days in Hospital | ||||||||||||||||
| 13 | no of days in ICU | ||||||||||||||||
| 14 | no of days in ward | ||||||||||||||||
| 15 | Nutritional Requirement | Kcal | Protein | Remarks | |||||||||||||
| 16 | No of Days of Different Type of Diet | NPO | Oral | Enteral | parenteral | ||||||||||||
| 17 | TIMEOF FIRST FEED | ||||||||||||||||
| 18 | Nutritional Intervention | First 12 Hour | 2nd 12 Hour | 2nd Day | 3rd DAY | 4th DAY | 5th DAY | 6thDAY | 7th DAY | ||||||||
| 19 | R | G | R | G | R | G | R | G | R | G | R | G | R | G | R | G | |
| 20 | TYPE Of DIET NPO/ORAL /ENTERAL/PARENTERAL | ||||||||||||||||
| 21 | REMARKS | ||||||||||||||||
| 22 | AMOUNT OF FEED | ||||||||||||||||
| 23 | NAME OF FORMULA | ||||||||||||||||
| 24 | NO OF SCOOP | ||||||||||||||||
| 25 | FREQUENCY | ||||||||||||||||
| 26 | NO OF FEED | ||||||||||||||||
| 27 | Kcal | ||||||||||||||||
| 28 | PROTEIN | ||||||||||||||||
| 29 | EXTRA | ||||||||||||||||
Findings:
| No of Days NPO | % of Patients Pre- Audit | % of Patients Post -Audit |
| 0 Days | 29.62% | 52.39% |
| 0.5 to 1 day | 56.79% | 42.1% |
| More than 1 days | 13.58% | 5.26% |
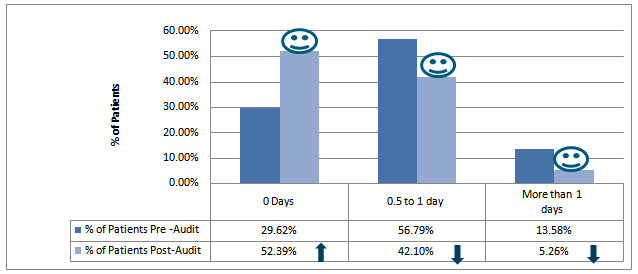
It was found that 56 .79% patients were kept NPO for one day and 13.58% patients were kept NPO more than one day. Only 29.62 % patients were not kept NPO. After taking corrective action % of patients who were not kept NPO increased 52.39%. And % of patients who were kept NPO 1 day and more than 1 day decreased respectively 42.10%, 5.26%.
Timing of first feed:
| First Feed Timings | % of Patients Pre- Audit | % of Patients Post -Audit |
| 0 to 12 hours | 38.26% | 63.14% |
| ˃12 hours to 24 hours | 43.2% | 26.3% |
| ˃ 24 Hours | 18.51% | 10.52% |

By giving feed in night time and starting feed in slow rate, there was a significant difference found in timing of first feed. % of patients who were get first feed with in first 24 hour after admission increases 81.5% to 89.5%.
First 24 hours to 7 Days Nutrition Consumption of Patients:
| Pre – Audit % of patients who were given | Post – Audit % of patients who were given | |||
| ≥ 80 % Required Kcal | ≥ 80 % Required protein | ≥ 80 % Required Kcal | ≥ 80 % Required protein | |
| Nutrition in first 24 hours | 12.34% | 12.34% | 50% | 50% |
| Nutrition in 2nd day to 7th day | 30.86% | 30.86% | 85% | 82% |

It was found that only 12% of patients who were able to get ≥ 80% of required kcal and protein in first 24 hour. This is improved by giving feed in night time and by straining feed early after admission and by giving continuous feed in place of bolus feeding.
It was difficult to keep all patients on continuous feeding because less no of pumps and costing issue with ready to hang formula feed. Combination of bolus and continuous feed gave a good result. Bolos feed was given to all patients if there was any feed missed due to investigations and other unavoidable reasons the gap was covered by giving continuous feed in night time. Because of these changes % of patients who were able to get≥ 80% of required kcal and protein in 2nd day to 7th day increased from 69% to 85% for calorie and 62.83% to 82% for protein.
Reason for Not Getting Required Nutrition:
- NPO for Procedure
- NPO for Radiological Diagnostics.
- Late order to start feed.
- Bolus feeding.
- No feeding in night time.
- Fluid restriction.
- Unawareness of RT feed protocol.
- Lack of nursing awareness regarding importance of nutrition.
- Un-availability and late supply of supplements.
- Un-availability of shakers for feed preparation.
Recommendations:
- No need to keep NPO for normal whole abdomen ultrasound.
- Can start feed from emergency as soon as possible, if there is no contraindication.
- Continuous feeding with slow rate (10ml-20ml/ hourly) can be started with in first 12 hours after admission.
- Prefer continuous feeding instead of bolus feeding.
- Feed can be given in night time to achieve nutritional goal.
- Training for nursing staff and duty doctors for RT feed protocol and procedure.
- If kept NPO for any procedure/test cover the feeding gap by giving feed in night time too.
Conclusions:
Over all study showed gap of nutritional intervention inspite of having updated international guidelines based SOP. Problem was found in implementation. It is very important to do the regular clinical nutritional audit to find out and minimize the reason/ factor of nutritional discrepancies. It is also important to do the small changes in process time to time to ease the implementation of the standard international guidelines.
REFERENCES:
- Mehta Y, et al.2018 Practice Guidelines for Nutrition in Critically Ill Patients: A Relook for Indian Scenario. Indian J Crit Care Med. 2018;22:263–273.
- ADA (American Dietetic Association). 2006. Critical illness evidence-based nutrition practice guideline.American Dietetic Association. http://www.adaevidencelibrary.com/topic.cfm?cat=2799 (accessed October 26, 2010).
- Mcilvoy, L., and K. Meyer. 2008. Nursing management of adults with severe traumatic brain injury. Glenview, IL: American Association of Neuroscience Nurses.
- Bratton, S. L., R. M. Chestnut, J. Ghajar, F. F. McConnell Hammond, O. A. Harris, R. Hartl, G. T. Manley, A. Nemecek, D. W. Newell, G. Rosenthal, J. Schouten, L. Shutter, S. D. Timmons, J. S. Ullman, W. Videtta, J. E. Wilberger, and D. W. Wright. 2007. Guidelines for the management of severe traumatic brain injury. XII. Nutrition. Journal of Neurotrauma 24(Suppl 1):S77–S82. [PubMed]
- Wilson RF1, Dente C, Tyburski J. 2001. The nutritional management of patients with head injuries.Neurol Res. 2001 Mar-Apr;23(2-3):121-8. [PubMed]
Author:
Ms. Shabista Nasreen, Consultant, Clinical Nutrition
Narayana Superspeciality Hospital, Guwahati, Assam.


Customer Reviews
Thanks for submitting your comment!